Blogs
Do you screen Spine in the presence of Shoulder Pain?

Shoulder Pain is considered to be one of the most commonly encountered problems in Musculoskeletal (MSK) area. Epidemiology suggests that nearly 10 to 16 per 100 patients suffer from shoulder pain (Winters et al; 99). Once present, it is proven to be persistent and recurrent, with 50% still unresolved after 18 months (Croft et al; 96). Thus suggesting that shoulder pain is one of the leading cause of referral to Physiotherapy (Winters et al; 99).
There are various ways by which clinicians diagnose Shoulder Pain. One of them is use of Ultrasound and Scans. Various changes like bursal thickening, AC Joint OA and Supraspinatus tendinosis in 96% of asymptomatic population (Girish et al; 14), and Rotator Cuff tears in nearly 65% of asymptomatic population (Mingawa et al; 13) has been noted. Another common method to diagnose shoulder pain is by using special tests. Poor accuracy and poor inter-rater reliability of various special tests has been shown (Hughes et al; 08, Gadogan et al; 11). Lack of uniformity in diagnostic labelling of shoulder pain, suggests use of an approach which relies on common characteristics that can easily be reproduced and are valid (Schellingerhout et al; 08). Majority of the times, cervical spine screening is not considered as a part of assessment for shoulder pain patients (Walker et al; 18) and this could affect the time of discharge (Abady et al’17), which could have a huge impact on shoulder pain epidemiology and its outcome.
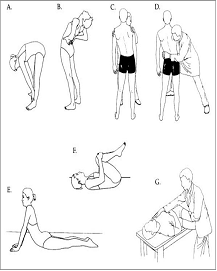
Mechanical Diagnosis and Therapy (MDT)/ McKenzie Method is the system of assessment and management, which utilises postures, positions and movements to classify patients into subgroups (McKenzie and May’00). In MDT, classification guides treatment. Primary aim/goal in the MDT system is screening of the spine in the presence of shoulder pain.
Cervical spine can give referred pain to shoulder (Menon & May’13; Bogduk’00). Various structures around the cervical spine could give pain across the shoulder. Using the MDT system, it is shown that nearly 1/3 rd of the shoulder pain originates from the cervical spine (Abady et al’17), implying the importance of screening the spine first. The reliability of classifying the patients with shoulder pain of cervical origin is excellent (Abady et al’14). The essence of the system is to give a direction specific exercise which brings lasting change in shoulder pain and all shoulder movements (Abady et al’17; Long et al’04). Here, if cervical spine is found to be the symptom generator for shoulder, the exercise is focused on cervical spine. It was also noted that the patients who demonstrated positive shoulder special tests during assessment, later, post directional specific cervical spine exercise demonstrated negative special tests for shoulder pain where the symptom generator was the cervical spine.
The McKenzie assessment and treatment system is a low technology, effective and valid tool that helps to differentially diagnose the shoulder and cervical sources of symptoms. The system may have a significant impact on the quality of life as well as health care utilization for majority of the patients with shoulder pain.
What is the effective way to diagnose Mechanical Low Back Pain?
Low Back Pain (LBP) is commonly encountered problem. Around 80-90% of population might have suffered from LBP at some point in their life (Raspe 1993). Research has shown that around 85% – 92% of LBP are mechanical in nature; means they are due to certain postures, positions, movements and functions and only 8%-15% are non-mechanical (Spitzer et al 1987; Hefford 2007). Hence most of LBP has non-specific cause and very few have specific. It seen that 80-90% of attacks of mechanical LBP recover in 6 weeks (Waddell 1987); but around 75% of them may not be symptom free at the end of even 1 year (Croft et al 1998), which tells us that disability due to LBP persists. Well, one should remember that LBP is a Symptom, not a diagnosis. Also, LBP is a recurrent problem, so as clinicians we should empower patients to control their own aches and pain.
Do I need to undergo MRI or CT scan to know the cause of my pain?
Well, despite the technological advances that have been made in recent years, we are still unable to identify the origin of LBP in majority of patients. Even the advanced imaging technology, such as Magnetic Resonance Imaging (MRI) or Computerised Axial Tomography (CAT) scan, our ability to identify the precise structure that generates symptoms and exact nature of the pathology affecting it remains limited (McKenzie and May 2003).

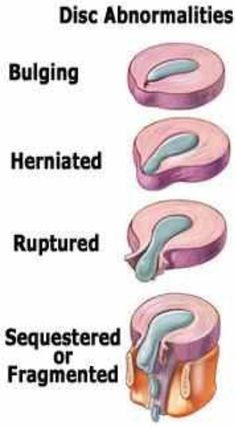
I’m worried, my scan shows I got prolapsed disc!!!
The prevalence of disk degeneration in asymptomatic individuals increased from 37% of 20-year-old individuals to 96% of 80-year-old individuals (Brinjikji et al 2014). Bulging or protruded discs have been found in over 50% of asymptomatic individuals (Jensen et al 1994; Weinreb et al 1989), those over 60 years 21% had spinal stenosis (Boden et al 1990). Also, patient knowledge of imaging findings do not alter outcome and are associated with a lesser sense of well-being (Ash et al 2008). Many imaging-based degenerative features are likely part of normal aging and may be unassociated with pain and routinely done yield little to no benefit (Karel et al 2015). Hence, there may be high chances of false-positive and false-negative findings.
My scan is normal; do I need to undergo invasive procedure to find the source of problem?

Some have highlighted the use of intra-articular or disc stimulating injections to find source of pain (Bogduk et al 1996), however these diagnosis rely upon invasive procedures involving significant exposure to x-rays, which are costly and require high level of skill. The Discogram is a reliable way to find disc as a source of symptoms, but its validity is still not proven (April 1992). Also it requires high skill and very costly.
What about McKenzie assessment and treatment?
As discussed earlier, mechanical LBP are due to certain postures, positions, movements and functions; it can rightly diagnosed and managed through certain postures, positions, movements and functions. The McKenzie method or Mechanical Diagnosis and Therapy (MDT) is one of the physical therapy approach which emphasizes on repeated end-range movements and positions to sub-group a patient in to different mechanical syndrome. The approach has been rigorously researched way round the world and is considered to be the most reliable and valid approach (Razmjou 2000, Kilpikosky 2002, Clare 2005). It allows the clinician to identify a patient who would respond to physical therapy or not; thus saving time and money of a patient. With this approach the clinician can rightly judge time of recovery the patient would take. It just does not focus only on pain, but also onto activity limitations. The best part of the method is it involves the patient himself to be a part of recovery process (Also called as Patient-Centered Approach) and thus making them independent to take control on their own pain; and managing future episode, if any. This is important because research has shown that LBP in particular has a tendency to recur and recurrences often occur with increased severity. Preventing recurrence is therefore more important than supplying short term relief through passive treatment. An important component of the assessment is that clinicians who are well trained in MDT are able to recognise patients with pathologies unsuitable for mechanical therapy such as Red flags, non-mechanical pathologies, which do requires investigations. These patients can be immediately referred for further medical evaluation to the appropriate specialist.
Hence, in many parts of world MDT is first line assessment process for many clinicians which is very safe and reliable way to find the mechanical and non-mechanical nature of LBP.